Why Colorectal Cancer Screening Starts at 45 Now
Five years ago, most people thought colonoscopy was something you did after turning 50. That changed in 2021. Major health groups - including the U.S. Preventive Services Task Force, the American Cancer Society, and the American College of Gastroenterology - all updated their guidelines to recommend starting screening at age 45. Why? Because colorectal cancer is rising fast in younger adults. Between 1995 and 2019, cases in people under 50 jumped by 2.2% every year. Rectal cancer, in particular, is climbing at 3.2% annually. This isn’t a fluke. It’s a trend. And it’s pushing doctors to act earlier.
Screening isn’t just about finding cancer. It’s about stopping it before it starts. Most colorectal cancers grow slowly from polyps - abnormal growths in the colon or rectum. If caught early, these polyps can be removed during a colonoscopy, cutting your risk of cancer by up to 67%. That’s not a small number. It’s life-changing.
Colonoscopy: The Gold Standard, But Not the Only Option
Colonoscopy is still the most effective screening tool. You lie down, get sedated, and a doctor uses a thin, flexible tube with a camera to look at your entire colon. If they find a polyp, they remove it right away. No extra visit. No waiting. That’s why it’s called the gold standard.
But it’s not perfect. You have to prep. That means drinking a large volume of laxative solution - often polyethylene glycol - the day before. Most people say the prep is worse than the procedure itself. A 2022 survey found 74% of patients called it the worst part. And while complications like perforation are rare (about 1 in 1,000), they do happen.
Still, the benefits outweigh the downsides. Studies show colonoscopy reduces colorectal cancer deaths by 65%. It’s also the only test that prevents cancer, not just detects it. That’s why experts still recommend it every 10 years for people at average risk.
Other Screening Tests: Less Invasive, But Different Trade-Offs
If colonoscopy feels too intimidating, you have options. The most common alternative is the fecal immunochemical test (FIT). It’s a simple at-home stool test that looks for hidden blood - a possible sign of cancer or large polyps. You do it once a year. No prep. No sedation. Just collect a sample and mail it in.
FIT is 79-88% accurate at finding cancer. But it misses smaller polyps. And if it comes back positive, you still need a colonoscopy to find out why. That’s a big limitation. In safety-net clinics, FIT has a 67% completion rate - way higher than colonoscopy’s 42%. It’s especially helpful for people who can’t take time off work, live far from hospitals, or fear the procedure.
Then there’s the multi-target stool DNA test (like Cologuard). It checks for both blood and DNA changes linked to cancer. It’s more sensitive - 92% for detecting cancer - but less specific. That means more false positives. About 13% of people get a positive result even when they don’t have cancer. That leads to unnecessary colonoscopies. It’s also more expensive and needs to be done every three years.
Other tests include flexible sigmoidoscopy (looks at only the lower colon, done every 5 years) and CT colonography (a virtual colonoscopy using X-rays). But neither can remove polyps. If something’s found, you still need a colonoscopy. Plus, CT scans expose you to radiation - about the same as a few chest X-rays.

Who Needs to Start Even Earlier Than 45?
If you have a family history of colorectal cancer or polyps, you’re not average risk. Same if you have inflammatory bowel disease (like Crohn’s or ulcerative colitis), or a genetic condition like Lynch syndrome or familial adenomatous polyposis (FAP). For these people, screening doesn’t wait until 45. It starts much earlier - sometimes in your 20s or 30s.
For example, if a parent was diagnosed with colon cancer before age 60, you should start screening at age 40 - or 10 years younger than their age at diagnosis, whichever comes first. If you have Lynch syndrome, you might need a colonoscopy every 1-2 years starting at 20-25.
African Americans are another high-risk group. They have a 20% higher incidence of colorectal cancer and 40% higher death rates than White Americans. That’s why the American College of Gastroenterology recommends they start screening at 45, even though others didn’t always follow that advice in the past. Now, it’s standard.
What Happens If Cancer Is Found?
Screening catches most cancers early - stage I or II. At that point, surgery alone can cure more than 90% of cases. But if the cancer has spread to lymph nodes or other organs (stage III or IV), you need chemotherapy.
For stage III colon cancer, the standard is a 6-month course of FOLFOX or CAPOX. FOLFOX combines oxaliplatin, leucovorin, and fluorouracil (5-FU). CAPOX uses capecitabine (an oral pill version of 5-FU) and oxaliplatin. Both are effective, but CAPOX lets you take most of the treatment at home. That’s a big perk for people who work or have family responsibilities.
Oxaliplatin can cause nerve damage - tingling or numbness in hands and feet. This can last months or even years. Some patients never fully recover. That’s why doctors now talk about “chemotherapy holidays” - stopping treatment after 3-4 months if the risk of recurrence is low and side effects are too much.
For stage IV (metastatic) cancer, treatment is different. It’s not about curing anymore - it’s about controlling. Drugs like cetuximab or bevacizumab are added to chemotherapy to block cancer growth signals. Genetic testing of the tumor is now routine. If the cancer has a KRAS or NRAS mutation, drugs like cetuximab won’t work. That’s why testing matters. It saves time and avoids useless side effects.
Real Stories, Real Outcomes
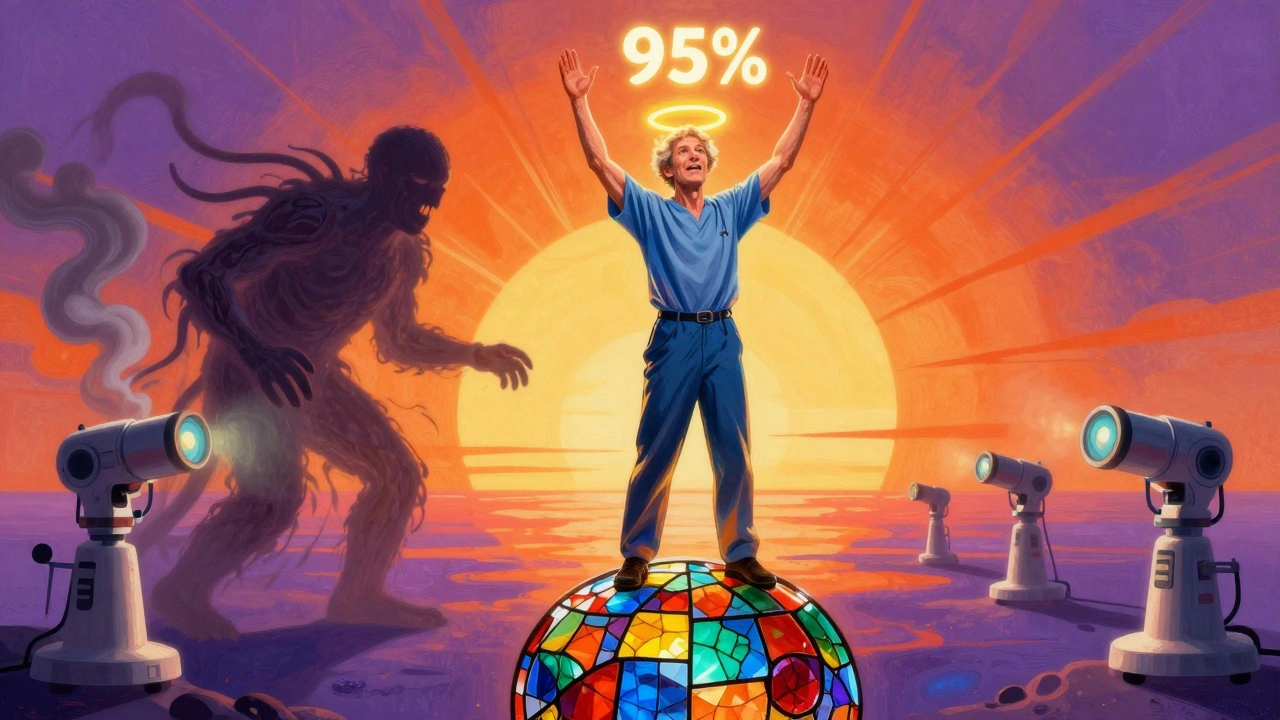
In 2023, a 47-year-old man in Georgia had his first colonoscopy at 45 - just because he heard the guidelines changed. The doctor found a small, early-stage tumor. He had surgery. No chemo. Five years later, he’s cancer-free. His survival chance? 95%.
Compare that to someone diagnosed at stage IV - the cancer has already spread to the liver. Their five-year survival? About 14%. That’s the gap between screening and no screening.
On Reddit, one user wrote: “I waited until I was 52 because I thought I was fine. Found stage III. Chemo wiped me out. I wish I’d done the colonoscopy at 45.”
These aren’t hypotheticals. They’re real people. And their outcomes hinge on timing.
Barriers to Screening - And How to Beat Them
Despite all the evidence, only 67% of adults aged 50-75 are up to date with screening. That’s below the national goal of 70.5%. Why? Cost, fear, lack of access, and poor communication.
Uninsured adults have a screening rate of just 58.4%. Privately insured? 78.2%. That’s a huge gap. Medicare covers colonoscopy with no out-of-pocket cost for most people. But many don’t know that.
Wait times are another problem. In rural areas, you might wait over 60 days just to get scheduled. Some clinics use patient navigators - staff who help you book tests, explain prep instructions, and follow up. Those clinics see 35% higher completion rates.
Automated reminders - texts or emails - boost adherence by 28%. Team-based care, where nurses or medical assistants handle prep education, cuts no-show rates by 42%.
What’s Next? Blood Tests and AI
Scientists are working on blood tests that detect DNA from colorectal tumors. The Guardant SHIELD test, tested in 10,000 people, found cancer with 83% accuracy. It’s not ready for prime time yet, but it could one day replace stool tests for people who won’t do either.
AI is already here. The GI Genius system, approved by the FDA in 2021, uses artificial intelligence to highlight polyps during colonoscopy. Studies show it increases detection by 14%. That means more early cancers caught - and fewer missed.
Future guidelines may one day personalize screening. Instead of everyone getting a colonoscopy every 10 years, your risk profile - based on genetics, diet, weight, and lifestyle - could determine how often you’re screened. Some might need it every 5 years. Others, every 15. That’s precision screening. And it’s coming.
What You Should Do Right Now
- If you’re 45 or older - schedule a colonoscopy or talk to your doctor about FIT.
- If you’re under 45 but have a family history - don’t wait. Ask about early screening.
- If you’ve had a polyp removed - follow your doctor’s advice on when to return. Surveillance intervals vary.
- If you’re over 75 - talk to your doctor. Screening may still make sense if you’re healthy and life expectancy is over 10 years.
- If you’re scared of the prep - ask about low-volume options or split-dose regimens. They’re easier.
Colorectal cancer is preventable. But only if you act. The clock doesn’t stop at 50 anymore. It starts at 45.


Elizabeth Grace
December 3, 2025 AT 11:59Steve Enck
December 3, 2025 AT 16:33Jay Everett
December 4, 2025 AT 07:19Ella van Rij
December 5, 2025 AT 16:05ATUL BHARDWAJ
December 7, 2025 AT 13:20Steve World Shopping
December 9, 2025 AT 03:41dave nevogt
December 10, 2025 AT 10:29Arun kumar
December 10, 2025 AT 11:25Zed theMartian
December 12, 2025 AT 02:05Alicia Marks
December 13, 2025 AT 16:06Paul Keller
December 14, 2025 AT 21:46