HSS-PH Pressure Estimator
Estimate Pulmonary Pressure
This tool estimates pulmonary artery pressure based on left ventricular outflow tract (LVOT) gradients. The relationship between LVOT obstruction and pulmonary hypertension is described in the article.
Understanding the Relationship
In HSS, LVOT obstruction forces the left ventricle to generate higher systolic pressures, which can transmit backward to the pulmonary circulation. The article explains that up to 15% of patients with severe LVOT gradients develop measurable pulmonary hypertension within five years.
This tool estimates pulmonary artery systolic pressure (PASP) based on the relationship described in the article: elevated left ventricular pressures can lead to pulmonary venous hypertension, which is reflected in increased pulmonary artery pressure.
Key Findings
Normal PASP: 20-35 mmHg
Mild PH: 35-45 mmHg
Moderate PH: 45-60 mmHg
Severe PH: >60 mmHg
Diagnostic Threshold: Mean pulmonary artery pressure (mPAP) ≥ 25 mmHg at rest.
Important Note
This calculator estimates pulmonary artery pressure based on clinical relationships described in the article. It should not be used as a substitute for clinical evaluation or diagnostic testing.
Estimated Results
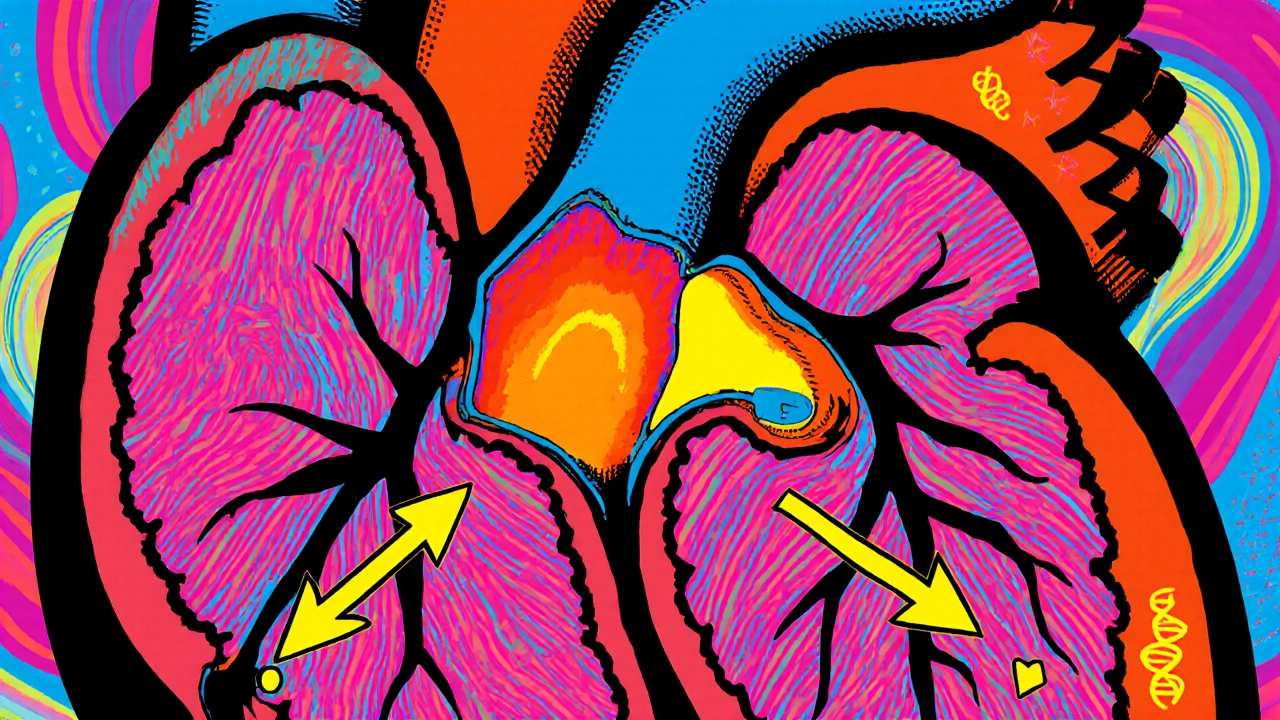
When the heart muscle grows too thick around the outflow tract, the resulting blockage can ripple into the lungs and cause a separate set of problems. Hypertrophic Subaortic Stenosis is a form of hypertrophic cardiomyopathy where the thickened septum narrows the left ventricular outflow tract (LVOT), creating a pressure gradient that the left ventricle must overcome to pump blood. Pulmonary Hypertension is a chronic elevation of pressure in the pulmonary arteries that strains the right side of the heart. Although they affect opposite chambers, a cascade of hemodynamic changes can link the two conditions.
Understanding Hypertrophic Subaortic Stenosis
HSS typically presents in adolescents or young adults, but it can surface at any age. The disease stems from genetic mutations-most often in the MYH7 or MYBPC3 genes-that cause myocyte disarray and septal hypertrophy. The hallmark feature is Systolic Anterior Motion (SAM) of the mitral valve leaflets, which further narrows the LVOT during systole. This obstruction creates a dynamic pressure gradient, measured in millimeters of mercury (mmHg) during an echocardiogram.
- Typical resting gradient: 30-50 mmHg; may exceed 100 mmHg with exercise.
- Symptoms: shortness of breath, chest pain, syncope, and palpitations.
- Key diagnostic tools: Doppler echocardiography, cardiac MRI, and genetic testing.
Effective treatment aims to reduce the gradient and alleviate symptoms. Beta‑blockers, non‑dihydropyridine calcium channel blockers, and disopyramide are first‑line pharmacologic options. In refractory cases, septal reduction therapy-either surgical myectomy or alcohol septal ablation-removes the obstructive tissue.
What Drives Pulmonary Hypertension?
PH is classified into five groups by the World Health Organization; the form most relevant to HSS belongs to Group 2-pulmonary venous hypertension due to left‑heart disease. When left‑ventricular filling pressures rise, blood backs up into the left atrium and pulmonary veins, leading to vascular remodeling, increased pulmonary arterial pressure, and eventually right‑ventricular (RV) overload.
- Diagnostic threshold: mean pulmonary arterial pressure (mPAP) ≥ 25 mmHg at rest.
- Symptoms: exertional dyspnea, fatigue, peripheral edema, and right‑sided chest discomfort.
- Key tests: right‑heart catheterization, transthoracic echocardiography, and lung function testing.
Treatment varies by PH group. For Group 2, the focus is on optimizing left‑heart function-often with diuretics, ACE inhibitors, or angiotensin‑receptor blockers-rather than employing pulmonary vasodilators that could worsen pulmonary edema.
How HSS Can Seed Pulmonary Hypertension
The link hinges on pressure transmission from the left to the right side of the heart. In HSS, the LVOT obstruction forces the left ventricle to generate higher systolic pressures. Over time, the following chain reaction can develop:
- Increased left‑ventricular end‑diastolic pressure (LVEDP) due to impaired outflow.
- Elevated left atrial pressure as the left ventricle struggles to empty.
- Back‑pressure into the pulmonary veins, raising pulmonary capillary wedge pressure.
- Chronic pulmonary venous congestion triggers endothelial dysfunction and smooth‑muscle proliferation, inching the pulmonary arteries toward hypertension.
- Right‑ventricular pressure overload leads to right‑heart failure if untreated.
Clinical studies from 2022‑2024 show that up to 15 % of patients with severe LVOT gradients develop measurable PH within five years, underscoring the physiological bridge between the two diseases.

Shared Pathophysiology: Remodeling and Neuro‑hormonal Activation
Both conditions involve myocardial remodeling and neuro‑hormonal cascades. Elevated wall stress in HSS stimulates the renin‑angiotensin‑aldosterone system (RAAS) and increases endothelin‑1 levels-both potent vasoconstrictors. Endothelin‑1 also drives pulmonary arterial smooth‑muscle proliferation, accelerating PH.
Conversely, chronic PH raises right‑ventricular afterload, which can shift the interventricular septum toward the left ventricle during diastole, worsening LVOT obstruction-a vicious feedback loop.
Diagnosing the Overlap: Imaging and Hemodynamics
Accurate diagnosis requires a blended approach that captures both left‑ and right‑sided pressures.
- Echocardiography remains the frontline tool. It quantifies LVOT gradients, assesses SAM, estimates pulmonary artery systolic pressure via tricuspid regurgitation velocity, and visualizes RV size.
- Cardiac MRI offers high‑resolution tissue characterization, revealing fibrosis that predicts adverse outcomes.
- When non‑invasive data are incongruent, right‑heart catheterization provides direct mPAP, pulmonary capillary wedge pressure, and cardiac output measurements.
Combining these modalities helps differentiate isolated HSS from HSS‑induced PH and guides therapy.
Management Strategies for Patients With Both Conditions
Therapeutic goals revolve around relieving LVOT obstruction, lowering left‑heart filling pressures, and preventing right‑heart strain.
- Pharmacologic relief of obstruction: Beta‑blockers (e.g., propranolol) reduce contractility, slowing SAM and lowering gradients. Non‑dihydropyridine calcium channel blockers (verapamil) offer similar benefits.
- Volume management: Low‑dose loop diuretics manage pulmonary congestion without compromising preload needed for LVOT gradients.
- RAAS inhibition: ACE inhibitors or ARBs blunt neuro‑hormonal activation, improving both left‑ and right‑ventricular compliance.
- Septal reduction therapy: In patients with refractory gradients (>70 mmHg) and concurrent PH, myectomy can dramatically reduce left‑sided pressures, indirectly lowering pulmonary pressures.
- Targeted pulmonary vasodilators: In select cases where PH persists despite optimal left‑heart therapy, phosphodiesterase‑5 inhibitors (sildenafil) may be added cautiously, monitoring for pulmonary edema.
Clinical guidelines (2023 ESC/ERS) recommend a stepwise approach: first optimize left‑heart disease, then consider PH‑specific agents only if WHO Group 2 criteria are not met.
Monitoring and Prognosis
Regular follow‑up is essential. Suggested schedule:
- Every 6 months: clinical assessment, ECG, and transthoracic echo.
- Annually: cardiac MRI to track fibrosis and ventricular volumes.
- When symptoms worsen: repeat right‑heart catheterization to reassess mPAP and pulmonary capillary wedge pressure.
Prognostic markers include:
- Peak LVOT gradient > 70 mmHg.
- mPAP ≥ 30 mmHg despite optimal left‑heart therapy.
- RV fractional area change < 35 % on echo.
Patients who achieve gradient reduction below 30 mmHg and maintain mPAP under 25 mmHg have survival rates similar to age‑matched controls, emphasizing the importance of early intervention.
Quick Comparison Table
| Aspect | Hypertrophic Subaortic Stenosis | Pulmonary Hypertension (Group 2) |
|---|---|---|
| Primary cause | Septal hypertrophy & LVOT obstruction | Elevated left‑heart filling pressures |
| Main hemodynamic effect | Increased LV systolic pressure gradient | Raised mean pulmonary arterial pressure |
| Typical symptoms | Dyspnea, chest pain, syncope | Exertional dyspnea, edema, fatigue |
| First‑line diagnostic tool | Doppler echocardiography (LVOT gradient) | Echocardiography (TR velocity) + right‑heart cath |
| Core treatment focus | Reduce obstruction (beta‑blocker, myectomy) | Optimize left‑heart function, diuretics |
| Shared pathophysiology | Neuro‑hormonal activation, endothelin‑1 rise | Endothelin‑1 mediated vascular remodeling |
Frequently Asked Questions
Can Hypertrophic Subaortic Stenosis cause pulmonary hypertension on its own?
Yes. Severe LVOT obstruction raises left‑ventricular pressures, which eventually back‑up into the pulmonary circulation and can trigger Group 2 pulmonary hypertension.
What echocardiographic signs suggest the development of PH in an HSS patient?
Key clues are an increased tricuspid regurgitation velocity (> 3.4 m/s), right‑atrial enlargement, and a flattening of the interventricular septum during systole.
Is alcohol septal ablation safe for someone who already has mild pulmonary hypertension?
Most studies report it’s safe if the PH is mild (mPAP < 30 mmHg) and the patient’s right‑ventricular function remains preserved. Careful hemodynamic monitoring is required.
Can pulmonary vasodilators like sildenafil worsen left‑heart obstruction?
They can raise pulmonary blood flow and, in rare cases, exacerbate pulmonary edema if left‑heart filling pressures are high. Use only after left‑heart pressures are controlled.
What lifestyle changes help both conditions?
Low‑salt diet, regular moderate aerobic exercise (under cardiology guidance), avoidance of stimulants, and strict blood‑pressure control are beneficial for HSS and reduce PH progression.

Don Goodman-Wilson
October 22, 2025 AT 18:53Oh great, another fancy heart jargon parade, as if we needed more reasons to hate modern medicine.
Bret Toadabush
October 23, 2025 AT 11:33Look, the pharma giants love pumping out these specialist articles to keep us buying endless pills. They hide the simple truth: lifestyle beats any drug. The whole LVOT gradient talk is just a distraction from the real cause-poor diet and stress. Wake up before they sell you another beta‑blocker.
Sarah Riley
October 24, 2025 AT 04:13Current hemodynamic models suggest that elevated LVEDP directly correlates with pulmonary capillary wedge pressure, implicating a mechanistic conduit for PH development in HSS.
Tammy Sinz
October 24, 2025 AT 20:53The interventricular septal shift during diastole exemplifies the bidirectional influence; mitigating SAM can thus indirectly attenuate RV afterload. Consider early beta‑blockade combined with careful volume management to break the feedback loop.
Christa Wilson
October 25, 2025 AT 13:33Love the thorough breakdown! 😊 Stay hopeful, management is getting better every day.
John Connolly
October 26, 2025 AT 05:13When tackling patients who present with both hypertrophic subaortic stenosis and secondary pulmonary hypertension, a systematic, stepwise protocol is essential. First, confirm the severity of LVOT obstruction using Doppler echocardiography, quantifying gradients both at rest and under provocation. If the resting gradient exceeds 70 mmHg, initiate pharmacologic therapy with negative inotropes such as beta‑blockers or non‑dihydropyridine calcium channel blockers to blunt contractility and reduce SAM. Simultaneously, assess volume status; low‑dose loop diuretics can alleviate pulmonary congestion without compromising preload needed for gradient reduction. Next, evaluate the response after several weeks – a meaningful drop in gradient (below 30 mmHg) often translates to a concomitant reduction in estimated pulmonary artery systolic pressure. Should gradients remain refractory, refer the patient for septal reduction therapy; surgical myectomy typically offers the most durable hemodynamic relief, while alcohol septal ablation provides a less invasive alternative for select anatomies. Importantly, after any septal reduction, re‑measure pulmonary pressures; many patients exhibit a notable decline in mPAP, underscoring the causal link between LVOT obstruction and Group 2 PH. If pulmonary hypertension persists despite optimized left‑heart management, a cautious trial of phosphodiesterase‑5 inhibitors may be justified, but only under strict hemodynamic monitoring to avoid pulmonary edema. Throughout this process, adhere to guideline‑directed medical therapy for heart failure, including ACE inhibitors or ARBs to temper neuro‑hormonal activation. Regular follow‑up is paramount: schedule six‑monthly clinical assessments with ECG and transthoracic echo, and obtain an annual cardiac MRI to monitor fibrosis and ventricular remodeling. Should symptoms worsen or new right‑ventricular dysfunction emerge, proceed to right‑heart catheterization for definitive pressure measurements. Finally, educate patients on lifestyle modifications-low‑salt diet, moderated aerobic activity, and avoidance of stimulants-to support pharmacologic and procedural interventions. By integrating imaging, hemodynamics, and tailored therapy, clinicians can markedly improve survival and quality of life for this complex cohort.
Tim Blümel
October 26, 2025 AT 21:53Spot‑on synthesis! 🎯 Your stepwise outline captures both the art and science of treatment. The emphasis on re‑evaluating mPAP post‑myectomy is especially valuable. Keep sharing these gems, they guide us through nuanced cases.
Joanne Ponnappa
October 27, 2025 AT 14:33Thanks for the clear summary, very helpful.
Emily Collins
October 28, 2025 AT 07:13Honestly, it feels like the heart’s playing a twisted game of tug‑of‑war, and we’re just watching the drama unfold.
Harini Prakash
October 28, 2025 AT 23:53The interplay between LVOT obstruction and pulmonary pressures really highlights how interconnected our cardiac chambers are. Incorporating both echo and MRI gives a comprehensive view, while right‑heart cath remains the gold standard for definitive diagnosis. I also appreciate the reminder about lifestyle tweaks-they’re often overlooked but can make a measurable difference. For clinicians in resource‑limited settings, focusing on echo‑derived gradients and tricuspid regurgitation velocity can still provide actionable insight. Ultimately, a patient‑centered approach that blends data with empathy yields the best outcomes.
Rachael Turner
October 29, 2025 AT 16:33Interesting point about neuro‑hormonal activation its role is undeniable yet often underappreciated we need more research on endothelin blockers in this niche group also consider patient quality of life when choosing aggressive interventions
Suryadevan Vasu
October 30, 2025 AT 09:13Optimizing preload while reducing LVOT gradient remains the cornerstone of therapy for preventing secondary pulmonary hypertension.