What Is Cervical Myelopathy?
Cervical myelopathy is a condition where the spinal cord in the neck becomes compressed, leading to nerve damage and loss of function. It’s not just neck pain or stiffness-it’s when the spinal cord itself is injured, often because the spinal canal has narrowed over time. This narrowing is called cervical spinal stenosis, and it’s the most common cause of cervical myelopathy. Most cases are due to wear and tear, known as cervical spondylotic myelopathy (CSM), which affects about 9% of people over 70. It’s the leading cause of spinal cord problems in adults over 55.
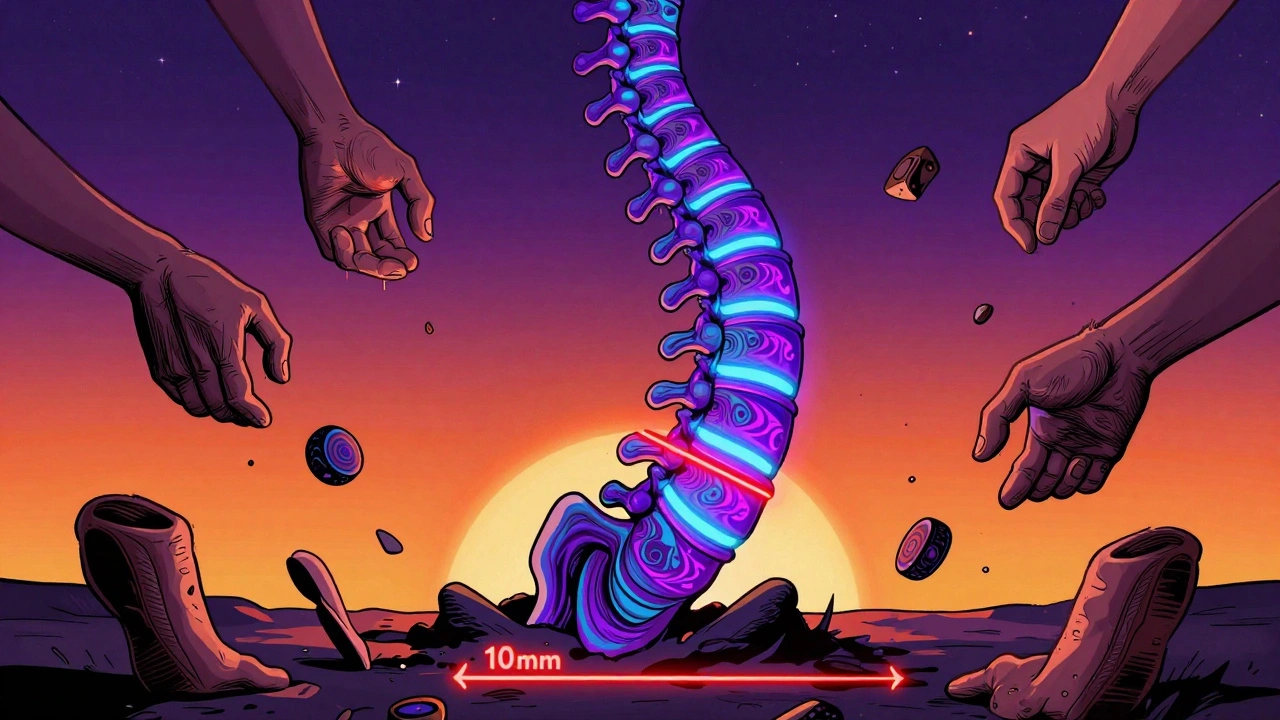
How Does Spinal Stenosis Lead to Myelopathy?
Spinal stenosis means the space around your spinal cord has shrunk. In a healthy neck, the spinal canal is about 17-18mm wide. When it drops below 13mm, it’s considered stenotic. Below 10mm, it’s severe. This narrowing happens slowly, often over decades, due to several changes:
- Discs lose water and flatten, pushing into the canal
- Facet joints grow larger from arthritis
- The ligamentum flavum (a ligament in the spine) thickens by 1-3mm
These changes don’t just squeeze the cord-they press on key nerve pathways. The corticospinal tracts, which control voluntary movement, get damaged. So do the spinocerebellar tracts, which help your brain know where your limbs are in space. That’s why people with cervical myelopathy often feel clumsy with their hands or unsteady on their feet.
What Are the Early Warning Signs?
Many people ignore early symptoms, thinking it’s just aging. But these signs are red flags:
- Hand clumsiness-dropping things, struggling to button shirts, or writing poorly
- Gait problems-feeling like your feet are stuck to the floor, tripping more often
- Balance issues-needing to hold onto walls or railings when walking
- Numbness or tingling in hands, arms, or legs
- Increased reflexes in knees and ankles (something a doctor checks with a reflex hammer)
These symptoms show up in about 70% of patients before they even feel neck pain. In fact, only half of people with cervical myelopathy report neck or arm pain. The real problem is the nerve damage, not the discomfort.
When Does It Get Worse?
Cervical myelopathy doesn’t always get worse the same way. About 45% of people see a slow, steady decline over 2-5 years. Another 30% hit a plateau and stay stable. But 25% get worse quickly-within 6 to 12 months. That’s why waiting to act can be dangerous.
Left untreated, symptoms can progress to:
- Loss of bladder or bowel control
- Severe weakness in arms or legs
- Paralysis below the level of compression
Studies show that 20-60% of people with untreated cervical myelopathy will suffer major neurological decline within a few years. Only 10-15% get better on their own.
How Is It Diagnosed?
Diagnosis isn’t just about feeling pain. It requires proof of spinal cord damage. Doctors use two things:
- Clinical symptoms-like hand clumsiness, gait issues, and reflex changes
- Imaging-specifically an MRI
An MRI is the gold standard. It shows both the narrowing of the canal and signal changes inside the spinal cord, which confirm actual damage. X-rays can show bone spurs or disc collapse, but they can’t tell if the cord is injured. Up to 21% of people over 40 have stenosis on MRI but no symptoms. That’s why symptoms matter just as much as images.
Doctors also use the Japanese Orthopaedic Association (JOA) score, a 17-point scale that measures movement, sensation, and bladder control. A score below 14 means myelopathy is present.
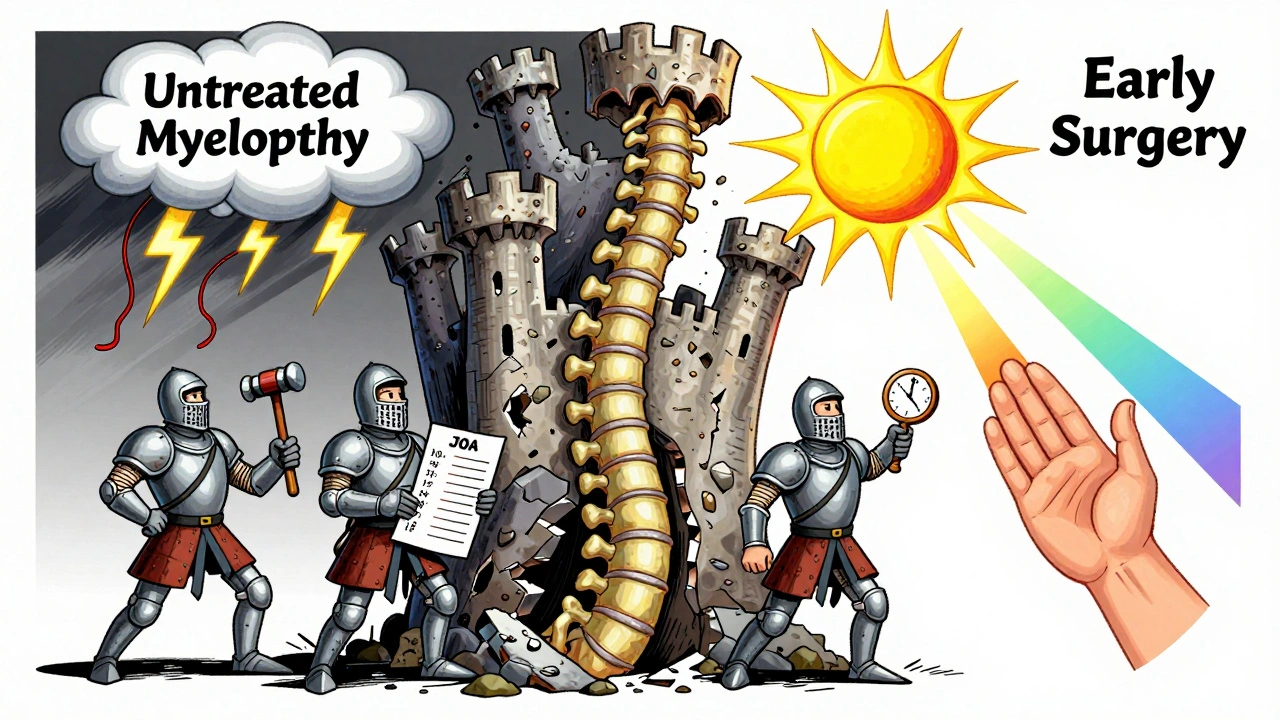
Can It Be Treated Without Surgery?
For very mild cases-JOA score 12-14-some doctors try conservative treatment: physical therapy, anti-inflammatory meds, activity changes. But the results aren’t great. Only 28% of patients improve over two years. More than half (63%) get worse.
Physical therapy helps maintain strength and balance, but it won’t reverse spinal cord damage. NSAIDs might reduce inflammation around the cord, but they don’t take pressure off it. If your symptoms are getting worse, or if your MRI shows clear cord compression, waiting isn’t safe.
When Is Surgery Necessary?
For moderate to severe myelopathy-JOA score below 12-surgery is strongly recommended. The American Academy of Orthopaedic Surgeons gives this a Grade A recommendation based on high-quality studies. In one major trial, 72% of surgical patients improved neurologically after two years. Only 29% of those who didn’t have surgery did.
Delaying surgery reduces your chances of recovery. Patients who operate within six months of symptoms start showing better function than those who wait a year. Each month of delay cuts recovery potential by about 3%.
What Are the Surgical Options?
There are three main types of surgery, chosen based on where the compression is and how many levels are affected.
Anterior Approaches (From the Front)
These are common for one or two levels of compression.
- Anterior Cervical Discectomy and Fusion (ACDF): Removes the damaged disc and fuses the vertebrae. Success rate: 85-90% for neurological improvement. But 5-7% of patients develop new problems in nearby discs within 10 years.
- Cervical Disc Arthroplasty (artificial disc): Replaces the disc without fusion. Newer models like the M6-C, approved in 2023 for multi-level use, preserve neck motion. At 24 months, 81% of patients kept movement, compared to 63% with fusion.
Posterior Approaches (From the Back)
Used when compression affects multiple levels or when the spine is misaligned.
- Laminectomy with fusion: Removes the back part of the vertebrae and fuses the bones. Best for severe cases. Neurological recovery: up to 85%.
- Laminoplasty: Opens the back of the spine like a door instead of removing it. Less pain post-op, but slightly lower recovery rate (78%).
Combined Approaches
For complex cases with both front and back compression, surgeons may do both anterior and posterior procedures in one or two stages.
What Are the Risks?
Every surgery has risks:
- Difficulty swallowing (dysphagia)-affects up to 22% after anterior surgery, usually improves in 3 months
- C5 nerve palsy-weakness in the shoulder or arm, happens in 4-6% of cases
- Neurological worsening-rare, 1-2%
- Chronic neck pain-18-35% after posterior or fusion procedures
Surgeons who do more than 50 cervical procedures a year have 32% fewer complications. Experience matters.
What Happens After Surgery?
Recovery isn’t quick. Most patients stay in the hospital 1-3 days. Full recovery takes 3-6 months.
- Physical therapy is essential-85% of patients need 8-12 weeks of formal rehab
- Focus is on gait training, balance, and strengthening neck muscles
- Smokers have a 50% higher risk of failed fusion-quitting before surgery helps
- Diabetics with HbA1c under 7.0 cut infection risk from 8.5% to 3.2%
Outcomes vary. Eighty-two percent of patients report better hand function after surgery. But only 65% regain normal walking. Nearly 30% still need a cane or walker.
What’s New in Treatment?
Research is moving fast:
- Minimally invasive laminoplasty reduces blood loss by 65% and hospital stay by almost two days
- Clinical trials are testing riluzole, a drug that may protect nerves during surgery-early results show 12% better recovery
- Robotic-assisted surgery is being tested to improve precision and reduce revision rates from 10% to under 7%
- Genetic markers like COL9A2 polymorphisms may soon help predict who’s at risk for faster degeneration
But experts warn: surgery rates have jumped 33% since 2010, but patient selection hasn’t improved. About 15-20% of current procedures may be unnecessary.
What Should You Do If You Suspect Cervical Myelopathy?
Don’t wait. If you’re noticing:
- Hand clumsiness
- Walking differently
- Loss of fine motor skills
-see a spine specialist within weeks. The average time to diagnosis is 14 months. Many patients see three or more doctors before getting the right answer.
Get an MRI within 2-4 weeks of noticing neurological symptoms. Early action doesn’t just help-it can prevent permanent damage.

Emily Haworth
December 13, 2025 AT 16:28Tom Zerkoff
December 14, 2025 AT 12:36Yatendra S
December 15, 2025 AT 13:40Himmat Singh
December 16, 2025 AT 01:04kevin moranga
December 17, 2025 AT 15:51Alvin Montanez
December 18, 2025 AT 07:53